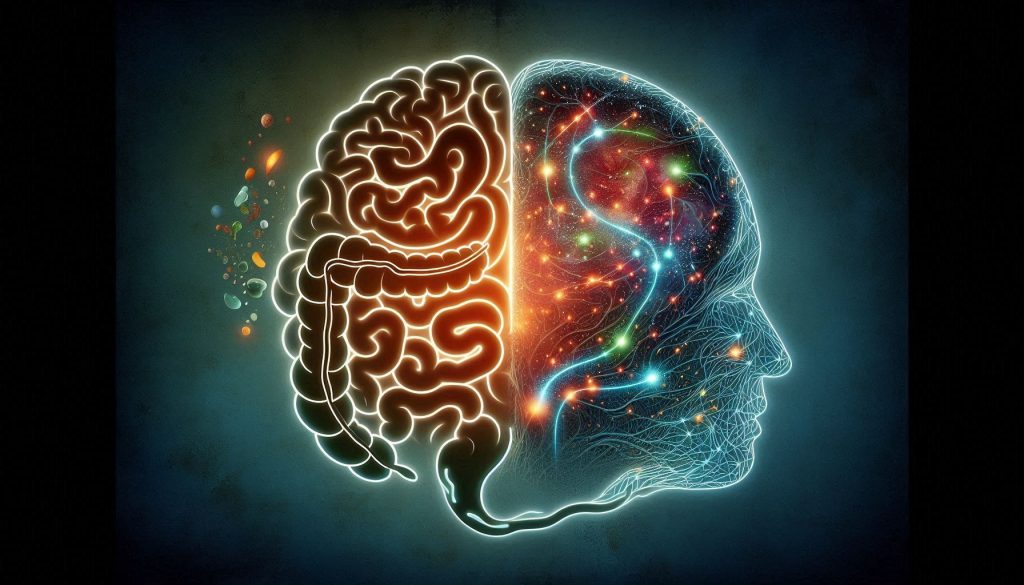
In recent years, the intricate relationship between our digestive system and mental health has garnered significant attention. Often referred to as the “gut-brain axis,” this complex communication network between the gastrointestinal tract and the brain has emerged as a vital area of study, particularly in the field of nutritional psychiatry. Scientists and healthcare professionals alike are beginning to uncover how profoundly our gut health can influence cognitive functions, mood regulation, and susceptibility to mental health disorders. Central to this relationship is the role of nutrition in modulating the gut micro biota, which in turn impacts brain function and emotional well-being. In this article, we delve deep into the science of the gut-brain axis, explore the mechanisms involved, and examine how dietary choices can be powerful tools in supporting mental health.
Understanding the Gut-Brain Axis
The gut-brain axis refers to the bidirectional communication system between the central nervous system (CNS) and the enteric nervous system (ENS), often dubbed the “second brain” due to its vast network of neurons. This axis encompasses neural, hormonal, and immunological signaling pathways, enabling the gut and brain to influence each other’s function.
A central component of this communication is the vague nerve, the longest cranial nerve in the body, which serves as a direct line connecting the brainstem to various organs, including the digestive tract. Through this nerve, the brain can modulate digestive processes, and the gut can send signals that influence mood and behavior. Additionally, the gut produces and responds to various neurotransmitters such as serotonin, dopamine, and gamma-amino butyric acid (GABA), all of which play crucial roles in mood regulation.
The Micro biota: Your Internal Ecosystem
Our gut is home to trillions of microorganisms, collectively known as the gut micro biota. These include bacteria, viruses, fungi, and other microbes that coexist in a symbiotic relationship with the human host. The gut micro biota is not merely a passive inhabitant; it actively contributes to nutrient metabolism, immune system modulation, and the maintenance of intestinal barrier integrity.
The composition of the gut micro biota is highly dynamic and influenced by numerous factors including genetics, mode of birth (vaginal vs. cesarean), breastfeeding, antibiotic use, environment, and, most significantly, diet. A diverse and balanced micro biota is considered essential for optimal health, whereas symbiosis, or microbial imbalance, has been linked to various physical and mental health disorders.
Nutrition’s Role in Shaping Gut Health
Diet is arguably the most modifiable factor influencing the gut micro biota. Macronutrients such as fats, proteins, and carbohydrates all impact microbial composition differently. Diets rich in fiber, fruits, vegetables, and whole grains tend to promote a diverse and resilient micro biota. These foods act as prebiotics, nourishing beneficial gut bacteria and enhancing the production of short-chain fatty acids (SCFAs), which have anti-inflammatory and neuroprotective properties.
On the other hand, high intake of saturated fats, refined sugars, and processed foods can promote the growth of pathogenic bacteria and contribute to inflammation and metabolic deregulation. Artificial sweeteners, commonly used in diet products, have also been shown to disrupt gut microbial balance.
Gut Health and Mental Health Disorders
The influence of gut health on mental health is supported by a growing body of research linking symbiosis to conditions such as depression, anxiety, autism spectrum disorder (ASD), and even neurodegenerative diseases like Alzheimer’s and Parkinson’s.
In depression and anxiety, studies have found altered gut micro biota profiles, often characterized by reduced microbial diversity and increased pro-inflammatory bacteria. These changes can lead to heightened inflammation, altered neurotransmitter production, and impaired stress response, all of which contribute to mood disorders.
In ASD, emerging evidence suggests that gut microbial imbalances may influence neurodevelopment and behavior. Children with autism often exhibit gastrointestinal issues and distinct micro biota profiles compared to neurotypical peers.
In the context of neurodegenerative diseases, chronic inflammation originating in the gut is believed to exacerbate neuronal damage and cognitive decline.
Mechanisms Linking Gut and Brain
Several biological pathways mediate the gut-brain connection:
- Neurotransmitter Production: Gut microbes synthesize neurotransmitters such as serotonin (about 90% of which is produced in the gut), dopamine, and GABA, directly affecting mood and cognition.
- Immune System Modulation: The gut is a major immune organ. Microbial balance influences systemic inflammation, which in turn affects brain health.
- Short-Chain Fatty Acids (SCFAs): Produced by fermentation of dietary fibers, SCFAs like butyrate support gut barrier integrity and have anti-inflammatory effects in the brain.
- Leaky Gut: Increased intestinal permeability allows harmful substances to enter the bloodstream, triggering systemic inflammation and potentially contributing to neuroinflammation.
Dietary Patterns and Mental Well-being
Certain dietary patterns have been associated with better mental health outcomes:
- Mediterranean Diet: Rich in fruits, vegetables, legumes, nuts, fish, and olive oil, this diet is linked to reduced risk of depression and cognitive decline. Its anti-inflammatory and antioxidant properties benefit both gut and brain.
- Western Diet: High in processed foods, sugars, and saturated fats, it is associated with increased risk of mental health disorders, likely due to its pro-inflammatory effects and negative impact on micro biota.
- Plant-Based Diets and Fermented Foods: Emerging evidence suggests these diets support microbial diversity and enhance gut-brain communication.
Psychobiotics: The Future of Mental Health Treatment?
Psychobiotics are a class of probiotics and prebiotics that have mental health benefits. These compounds modulate the micro biota in ways that positively affect mood, anxiety, and cognitive function.
Probiotics such as Lactobacillus and Bifid bacterium strains have been shown in clinical trials to reduce symptoms of depression and anxiety. Prebiotics like inulin and galactooligosaccharides (GOS) stimulate the growth of beneficial bacteria. Postbiotics, or metabolic byproducts of probiotics, also show promise in modulating brain function.
Though still in its infancy, the field of psychobiotics represents a promising avenue for integrative approaches to mental health care.
Lifestyle Factors and the Gut-Brain Axis
Beyond diet, several lifestyle factors influence the gut-brain connection:
- Sleep: Poor sleep disrupts microbial rhythms and increases inflammation.
- Stress: Chronic stress alters gut micro biota composition and permeability.
- Exercise: Regular physical activity enhances microbial diversity and brain health.
- Antibiotic Use: While sometimes necessary, antibiotics can disrupt micro biota balance; recovery strategies include probiotics and fiber-rich foods.
- Early Life Factors: Birth method, breastfeeding, and early diet influence lifelong micro biota development and brain health.
Clinical Implications and Future Research
Personalized nutrition, which tailors dietary interventions to an individual’s unique gut micro biota profile, is emerging as a revolutionary approach in the field of nutritional psychiatry. This burgeoning area of study leverages advances in micro biome sequencing, metabolomics, and computational modeling to provide insights into how the gut’s microbial ecosystem influences mental health. As our understanding of the gut-brain axis continues to expand, researchers are increasingly able to design precision diets that cater to the specific needs of individuals, thus optimizing both their physical and mental well-being. The concept of personalized nutrition involves analyzing an individual’s gut micro biota composition, understanding the balance of beneficial and pathogenic microbes, and then recommending dietary adjustments that support microbial diversity and brain health.
One of the primary driving forces behind the rise of personalized nutrition is the growth of micro biome sequencing technologies. High-throughput DNA sequencing techniques now allow for the identification and analysis of trillions of microorganisms within the gut, providing valuable data on the microbial composition and its functional capacity. Furthermore, metabolomics, which involves the study of metabolites produced by the micro biota, offers deeper insights into how these microorganisms influence human metabolism, neurotransmitter production, and systemic inflammation. With these technologies, researchers can pinpoint specific microbes or metabolic byproducts that are associated with various mental health conditions, such as depression, anxiety, and cognitive decline. This enables clinicians to recommend more precise dietary strategies aimed at fostering a healthier micro biome, thereby improving mental health outcomes.
In addition to individual-specific interventions, nutritional psychiatry is becoming increasingly recognized as a promising field for preventing and treating mental health disorders. Studies have shown that dietary patterns, particularly those rich in whole foods, fiber, and fermented products, can positively impact mood and cognitive function. However, despite the promising results, the field faces several challenges. One of the most significant hurdles is the high degree of variability in micro biome responses across different individuals. What works for one person’s micro biota might not work for another, making it difficult to establish universal guidelines for nutritional interventions. This variability underscores the importance of personalized, data-driven approaches to nutritional psychiatry.
Another critical challenge is the need for large-scale, longitudinal studies to further validate the long-term effects of dietary interventions on mental health. While there is a growing body of evidence supporting the link between gut health and mental well-being, much of the research remains preliminary. Long-term human trials that monitor the effects of diet and micro biome modulation on mental health are essential to fully understand the scope and limitations of these interventions. Additionally, more comprehensive studies are needed to examine how different environmental factors, such as stress, sleep, and lifestyle, interact with the micro biome to influence mental health.
Ethical considerations also play a crucial role in the evolution of nutritional psychiatry. Manipulating the micro biome, particularly in vulnerable populations such as children, the elderly, or those with severe mental health disorders, raises important questions about safety, consent, and equity. While the promise of personalized nutrition is exciting, there is a need for careful regulatory oversight to ensure that interventions are safe, ethical, and accessible to all. Furthermore, researchers and healthcare providers must be mindful of the potential for over-simplification or commercialization of micro biome-based therapies. As the field continues to grow, rigorous research, ethical frameworks, and clear regulatory guidelines will be essential in ensuring that micro biome-based dietary interventions are both effective and responsibly applied.
In conclusion, personalized nutrition based on individual micro biome profiles represents a promising frontier in nutritional psychiatry, with the potential to revolutionize mental health treatment. As technology continues to advance and the understanding of the gut-brain connection deepens, personalized dietary interventions will likely become more mainstream. However, the field must address challenges related to variability in micro biome responses, the need for large-scale studies, and ethical concerns to fully harness the potential of personalized nutrition in improving mental health outcomes.
Conclusion
The gut-brain connection underscores a revolutionary understanding of mental health: that our emotional and cognitive well-being is deeply intertwined with the health of our digestive system. Nutrition plays a foundational role in shaping this relationship, influencing the composition and activity of the gut micro biota, which in turn impacts brain function and mood.
As research continues to unravel the complexities of this axis, it becomes increasingly clear that dietary choices are not merely about physical health but are integral to our mental and emotional lives. By embracing a holistic approach that considers the gut as a key player in mental health, individuals and healthcare providers can unlock new pathways to psychological resilience and well-being.
SOURCES
Dina, T. G., & Cyan, J. F. (2017). The Micro biome-Gut-Brain Axis in Health and Disease. Gastroenterology Clinics of North America, 46(1), 77–89.
Mayer, E. A., et al. (2014). Gut Microbes and the Brain: Paradigm Shift in Neuroscience. Journal of Neuroscience, 34(36), 11808–11815.
Brick, P., et al. (2011). The Intestinal Micro biota and Brain Function. The American Journal of Gastroenterology, 106(11), 1253-1262.
Foster, J. A., & Neufeld, K. A. (2013). The Gut–Brain Axis: How the Micro biome Influences Anxiety and Depression. Trends in Neurosciences, 36(5), 305–312.
Collins, S. M., et al. (2012). The Gut Micro biome: A New Frontier in Neuroscience. The Journal of Physiology, 590(7), 1495-1502.
Clarke, G., et al. (2013). The Micro biome-Gut-Brain Axis during Early Life Regulates the Hippocampal Serotonergic System in the Rat. Molecular Psychiatry, 18(7), 718–725.
Carabotti, M., et al. (2015). The Gut-Brain Axis: Interactions between Enteric Micro biota, Central and Enteric Nervous Systems. Annals of Gastroenterology, 28(4), 203–209.
Zhao, L., et al. (2018). Gut Micro biota Composition Modulates the Efficacy of Antidepressant Treatment in Mouse Models of Depression. Scientific Reports, 8(1), 2670.
Mayer, E. A., et al. (2015). Gut Micro biota and Brain Function: The Gut-Brain Axis. Journal of Clinical Investigation, 125(3), 857–868.
Markel, J. G., et al. (2013). Sex Differences in the Gut Micro biome Drive Hormone-Dependent Regulation of Autoimmunity. Science, 339(6123), 1084–1088.
Ki colt-Glaser, J. K., et al. (2015). The Effects of Stress on the Immune System and Gut Micro biome. Current Opinion in Psychology, 5, 63–68.
Sparker, A., et al. (2016). Psychobiotics and the Manipulation of Bacteria–Gut–Brain Signals. Trends in Neurosciences, 39(11), 733–742.
Khan, A., et al. (2021). The Role of Gut Micro biota in Mental Health: A Systematic Review of Literature. The Journal of Psychiatric Research, 136, 5-14.
Vargas, A. P., et al. (2017). Role of the Micro biota in Mental Health: A Review of Literature. Frontiers in Neurology, 8, 3.
Hoban, A. E., et al. (2016). Regulation of Intestinal and Brain Serotonin by Short-Chain Fatty Acids. Frontiers in Molecular Neuroscience, 9, 1-7.
Kawabata, A., et al. (2016). Gut Micro biota and Psychiatric Disorders: A Review of Literature. International Journal of Environmental Research and Public Health, 13(11), 1112.
Meninges, R., et al. (2009). Impact of Probiotics on the Gut–Brain Axis. World Journal of Gastroenterology, 15(6), 673–679.
Grower, M. W., & Morgan, R. (2014). The Impact of Diet and the Gut Micro biome on Immune and Neurocognitive Function. Journal of Clinical Psychology, 70(1), 1–10.
Bravo, J. A., et al. (2011). Ingestion of Lactobacillus Strain modulates stress-related behavior and central GABA receptor expression in a mouse model of depression. Proceedings of the National Academy of Sciences, 108(38), 16050–16055.
Sharon, G., et al. (2016). Human Gut Micro biota and the Development of Parkinson’s disease. Frontiers in Neuroscience, 10, 888.
HISTORY
Current Version
April 11, 2025
Written By:
ASIFA



0 Comments