Aging is a deeply intricate biological process marked by gradual changes in organ function, hormone levels, nutrient metabolism, and body composition. As people age, the risk for chronic diseases such as hypertension, type 2 diabetes, arthritis, cardiovascular disease, osteoporosis, and neurodegenerative disorders like Alzheimer’s increases dramatically. With this rise in chronic health conditions comes a parallel surge in the use of pharmaceutical medications designed to manage symptoms, slow disease progression, and preserve quality of life. In fact, data from the National Center for Health Statistics (2022) reveals that nearly 90% of adults over the age of 65 take at least one prescription medication, while more than 40% take five or more medications daily, a phenomenon known as polypharmacy.
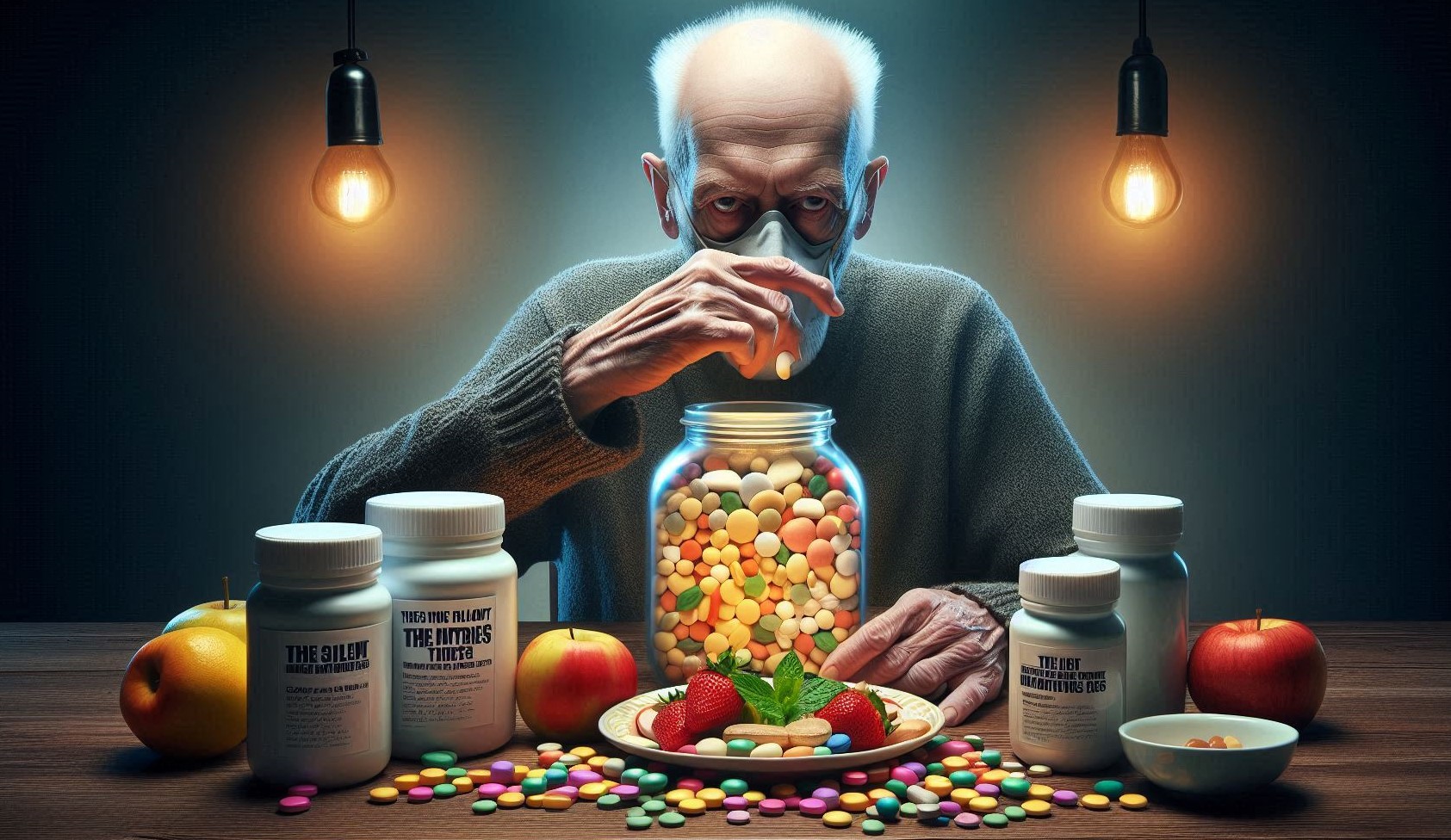
Medications are often essential for survival and symptom control, but beneath this therapeutic support lies a clinically under recognized problem: drug-induced nutrient depletion. These so-called “silent nutrient thieves” don’t announce themselves with loud side effects. Instead, they subtly undermine the nutritional foundation of an already vulnerable population—stealing away essential vitamins, minerals, and coenzymes that are critical for everything from cognitive clarity and immune defense to bone strength, energy production, and mood regulation.
Over time, these micronutrient losses accumulate, creating a cascade of subclinical deficiencies that may present with vague, nonspecific symptoms: persistent fatigue, irritability, forgetfulness, weakened immunity, frailty, or loss of muscle mass. These symptoms are often attributed to “normal aging,” delaying appropriate diagnosis and nutritional intervention. Even more concerning, such deficiencies can mimic or exacerbate the very conditions these medications are prescribed to manage—such as depression, neuropathy, or cardiovascular complications—leading to a potentially dangerous clinical loop of overmedication and undernourishment.
The elderly are uniquely susceptible to this phenomenon for several physiological and lifestyle-related reasons. With age, there is a decline in stomach acid production (hypochlorhydria), which impairs absorption of key nutrients like vitamin B12, calcium, iron, and magnesium. Liver and kidney function, both of which play central roles in nutrient metabolism and excretion, are often diminished. Appetite may decrease due to changes in taste, dentition issues, depression, or medication side effects—leading to lower intake of essential nutrients from food. Add to this the synergistic effects of multiple drugs that may simultaneously block absorption, alter metabolism, increase urinary excretion, or damage the micro biome, and it becomes clear why the elderly are at high nutritional risk even when they are under “good medical care.”
Consider some widely prescribed examples:
- Proton pump inhibitors (PPIs), used for acid reflux, impair vitamin B12, magnesium, calcium, and iron absorption.
- Motorman, a cornerstone of type 2 diabetes management, reduces vitamin B12 and foliates levels, increasing risk for neuropathy and anemia.
- Stations, the most prescribed lipid-lowering drugs, deplete Coenzyme Q10, potentially contributing to fatigue and muscle pain.
- Diuretics, common in heart failure and hypertension, cause the loss of potassium, magnesium, sodium, and thiamine.
- Corticosteroids, used for inflammatory conditions, rob the body of calcium, vitamin D, potassium, and zinc.
Despite decades of use, many clinicians remain unaware of these nutrient-depleting properties or fail to routinely screen for deficiencies unless symptoms are severe. This lack of recognition contributes to under diagnosed malnutrition in older adults, even those who appear medically stable.
In an era where preventive care, personalized medicine, and longevity science are gaining traction, it is essential to broaden the conversation around medication management to include nutritional stewardship. Recognizing the nutritional toll of pharmaceuticals is no longer optional—it is a clinical imperative. Nutrition should not be treated as a passive background variable but rather as a co-equal partner in drug therapy, especially in geriatrics.
This guide will explore in depth the medications most commonly associated with nutrient depletion, the biological mechanisms behind these losses, clinical signs that mimic aging, strategies for detection and correction, and the critical role that pharmacists, dietitians, and physicians must play in identifying and addressing these silent nutrient thieves before they compromise health, mobility, or independence in older adults.
Why Medication-Induced Nutrient Depletion Matters in Older Adults
Older adults are uniquely susceptible due to:
- Declining renal and hepatic function
- Reduced gastric acid secretion
- Altered gut micro biota
- Slower gastrointestinal motility
- Reduced dietary intake and appetite
Nutritional vulnerability is further compounded by polypharmacy, defined as the use of five or more medications. According to Maher et al. (2014), over 40% of older adults in the U.S. take five or more prescription drugs daily—magnifying the risk of depletion.
Age-Related Pharmacokinetics and Nutritional Vulnerability
Pharmacokinetics in the elderly shifts due to:
- Decreased albumin (affecting drug binding)
- Slower metabolism (Phase I and II detoxification)
- Altered body composition (↑ fat, ↓ lean mass)
- Delayed gastric emptying
These changes can extend drug half-life and heighten the body’s exposure, making nutrient loss more likely and recovery slower.
Commonly Used Medications That Deplete Nutrients
Diuretics (e.g., Furosemide, Hydrochlorothiazide)
- Nutrients depleted:
- Potassium
- Magnesium
- Sodium
- Calcium
- Zinc
- B-vitamins (especially B1)
- Mechanism:
- Diuretics increase urine output, flushing out water-soluble nutrients.
- Risks:
- Hypokalemia can lead to arrhythmias; thiamine deficiency can mimic heart failure symptoms (Weiss et al., 2017).
Proton Pump Inhibitors (e.g., Omeprazole, Pantoprazole)
- Nutrients depleted:
- Vitamin B12
- Magnesium
- Calcium
- Iron
- Zinc
- Mechanism:
- Gastric acid is essential for the ionization and absorption of minerals and B12 cleavage from food.
- Consequences:
- Pernicious anemia, cognitive decline, and increased fracture risk (Lam et al., 2013).
Motorman (for Type 2 Diabetes)
- Nutrients depleted:
- Vitamin B12
- Foliate
- Coenzyme Q10 (CoQ10)
- Mechanism:
- Inhibits B12 absorption in the terminal ileum.
- Clinical signs:
- Peripheral neuropathy, fatigue, memory issues—often misattributed to diabetes progression (de Jaeger et al., 2010).
Stations (e.g., Atorvastatin, Simvastatin)
- Nutrients depleted:
- CoQ10
- Vitamin D
- Selenium
- Mechanism:
- Inhibit the mevalonate pathway, which also produces CoQ10.
- Impact:
- Muscle pain, weakness, fatigue—CoQ10 supplementation may help mitigate stating-induced sympathy (Marc off & Thompson, 2007).
Antihypertensive (e.g., Beta Blockers, ACE inhibitors)
- Nutrients depleted:
- Zinc
- CoQ10
- Potassium
- Magnesium
- Notable:
- ACE inhibitors may increase zinc excretion, impacting immune health and taste perception (Song et al., 2012).
Laxatives
- Nutrients depleted:
- Potassium
- Magnesium
- Fat-soluble vitamins (A, D, E, K)
- Mechanism:
- Rapid transit time reduces nutrient absorption.
- Long-term use:
- Chronic depletion can lead to muscle cramps, arrhythmias, and fatigue.
Antidepressants & Antipsychotics (e.g., SSRIs, Risperidone)
- Nutrients affected:
- Sodium (hyponatremia)
- Foliate
- B6
- Magnesium
- Clinical concern:
- Low foliate worsens depression. Sodium imbalance increases fall risk (Alpert et al., 2016).
Antiepileptic (e.g., Phonation, Carbamazepine)
- Nutrients depleted:
- Vitamin D
- Calcium
- Folic acid
- Biotin
- B6
- Carnation
- Risk:
- Increased bone turnover, osteomalacia, cognitive symptoms (Pack, 2003).
Hormonal Medications (e.g., Corticosteroids)
- Nutrients depleted:
- Calcium
- Magnesium
- Vitamin D
- Zinc
- Potassium
- Notable:
- Long-term corticosteroid use is associated with osteoporosis and sarcopenia (Buckley et al., 2017).
Antibiotics
- Nutrients affected:
- Vitamin K (gut flora disruption)
- B-vitamins
- Magnesium
- Robotics (gut health)
Note:
Broad-spectrum antibiotics destroy commensally flora essential for nutrient synthesis (McFarland, 2005).
Nutrient Deficiencies by Drug Class: A Matrix
| Drug Class | Key Nutrients Depleted |
| Diuretics | Potassium, Magnesium, Thiamine |
| PPIs | B12, Magnesium, Calcium, Iron |
| Motorman | B12, Foliate, CoQ10 |
| Stations | CoQ10, Vitamin D |
| Antiepileptic | Vitamin D, Foliate, Biotin, Carnation |
| Antidepressants | Sodium, Foliate, B6 |
| Corticosteroids | Calcium, Vitamin D, Zinc |
Symptoms That Mimic Aging but Stem from Depletion
- Fatigue → B12, CoQ10, iron deficiency
- Cognitive decline → B12, foliate
- Muscle cramps → Magnesium, potassium
- Fractures → Vitamin D, calcium
- Taste loss → Zinc
- Falls and weakness → Sodium imbalance
Misdiagnosis is common, leading to unnecessary interventions instead of nutrient repletion.
Polypharmacy and the Compounding Effect
Polypharmacy increases nutrient theft exponentially. Drugs may:
- Interact synergistically in depleting a single nutrient (e.g., PPIs + motorman → severe B12 loss)
- Inhibit absorption and increase excretion simultaneously
- Mask symptoms of deficiency (e.g., corticosteroids masking inflammation from nutrient-related muscle breakdown)
The Role of Functional and Micronutrient Testing
Key tests include:
- Serum B12 and MMA (methylmalonic acid)
- RBC magnesium (not just serum)
- Homocysteine (for foliate/B12)
- 25(OH)D (Vitamin D)
- CoQ10 levels (for stating users)
Functional tests detect deficiencies before serum levels drop, offering a proactive window.
Food-Drug Interactions: Blocking Absorption
Some examples:
- Calcium binds with tetracycline’s, blocking antibiotic absorption.
- Grapefruit inhibits CYP3A4, increasing drug bioavailability.
- Fiber can impair levothyroxine absorption.
- Green leafy vegetables reduce warfare effectiveness (Vitamin K).
Counseling must account for meal timing, food types, and supplement interactions.
Repletion Strategies: Food First, Then Supplements
Food-first approach:
- Magnesium: Nuts, seeds, leafy greens
- B12: Meat, fish, dairy
- Foliate: Legumes, leafy greens
- CoQ10: Organ meats, sardines
- Potassium: Bananas, sweet potatoes
- Zinc: Oysters, pumpkin seeds
Supplements:
Tailored to:
- Degree of depletion
- Bioavailability (e.g., methylcobalamin vs. cyanocobalamin)
- Co morbidities (renal disease alters potassium/magnesium tolerance)
Collaboration between Dietitians, Pharmacists, and Physicians
Multidisciplinary teams should:
- Regularly review medication lists
- Order labs for at-risk nutrients
- Refer to dietitians for food-based correction
- Consider deprescribing when appropriate
Joint accountability prevents nutrient loss from falling through the cracks.
Special Populations
- Demential: Nutrient depletion mimics and may exacerbate cognitive decline.
- Frailty:Depletion → sarcopenia → immobility → further decline.
- Institutionalized Seniors:Often on 10+ medications, with limited food variety—highest risk group.
- Red Flags for Suspecting Drug-Induced Nutrient Loss
- Worsening cognition despite stable disease
- Unexplained fatigue
- Falls without known cause
- New depression in long-term PPI/stating users
- Recurrent infections (zinc, vitamin D deficiency)
Clinical Case Studies
- Case 1:An 81-year-old on omeprazole, motorman, and furosemide presented with falls, fatigue, and neuropathy. Labs revealed B12 <180 pg/mol and magnesium deficiency. Intervention led to resolution in 4 weeks.
- Case 2:A 74-year-old woman on corticosteroids developed fractures and insomnia. DEXA scan confirmed osteopenia; labs showed low vitamin D and calcium. Repletion reduced further bone loss.
Recommendations for Monitoring and Prevention
- Annual nutrient screening for high-risk meds
- Medication reconciliation every 6 months
- Encourage diversified, nutrient-dense diets
- Include pharmacists in geriatric care teams
- Use drug-nutrient interaction tools (e.g., Lexis-Interact)
Limitations in Current Practice and Research
- Drug inserts rarely warn of nutrient depletion
- Research focuses on acute side effects, not subtle chronic ones
- Nutrient testing is underutilized due to cost, lack of awareness
- Many clinicians are unaware of food-first repletion protocols
Future Directions and Innovations
- AI-assisted drug-nutrient interaction databases
- Wearable’s to detect functional deficiency signs early
- EMR alerts for nutrient-depleting meds
- Policy advocacy for mandatory nutrient interaction labeling
Patient Advocacy and Education
- Teach patients to ask about nutrient risks
- Provide accessible charts for food sources of common nutrients
- Support groups for stating fatigue or PPI withdrawal
Conclusion
As medicine continues to advance and human longevity increases, we are witnessing more people living into their 80s, 90s, and even past 100. However, longevity without vitality is a hollow victory. A longer life must be paired with functional health, autonomy, and nutritional resilience. Yet one of the most under-recognized barriers to achieving this goal is not just age itself, but the cumulative nutrient depletion caused by long-term medication use—especially in older adults who rely on multiple prescriptions to manage chronic illness.
Modern pharmacology has gifted us with remarkable tools to extend life and control disease, from blood pressure medications and stations to antidepressants, acid reducers, and anti-inflammatory. These drugs are often indispensable. But while they treat one issue, they may silently introduce another: progressive micronutrient depletion. This stealthy loss can gradually erode the very physiological systems we are trying to protect—undermining cognition, energy, muscle function, immune response, and even mood.
The tragedy is that this decline is often misinterpreted as a natural part of aging. A fatigued older adult may be seen as “just getting old,” when in fact they may be B12-deficient due to long-term PPI or motorman use. A frail, falling patient may not have dementia or muscle loss due to age, but rather vitamin D, magnesium, or potassium depletion from diuretics or corticosteroids. When nutrient theft goes unnoticed, it leads not only to unnecessary suffering but also to avoidable hospitalizations, fractures, disability, and loss of independence.
This is not an unsolvable problem. With better interdisciplinary collaboration between prescribers, pharmacists, and registered dietitians, medication regimens can be regularly evaluated for their nutritional impact. Screening protocols can be implemented for high-risk nutrients—such as B12, vitamin D, magnesium, and CoQ10—especially in patients taking known depleting drugs. Clinical awareness campaigns can empower healthcare professionals to look beyond symptoms and ask critical questions: “Could this fatigue be nutritional? Is this neuropathy from diabetes or from motorman-induced B12 loss?”
The answer lies in integrating nutrition into every step of pharmaceutical care—from the moment of prescribing, through monitoring, and in patient education. Nutritional repletion strategies—both food-based and supplemental—must become standard practice, not an afterthought.
Ultimately, the goal is not to vilify medications, but to reframe the conversation: Medications are lifesaving, but only when paired with the nutritional vigilance that sustains the body systems they aim to protect. In the pursuit of healthy aging, nutrient protection is not optional. It is essential. We must stop thinking of nutrient depletion as a rare exception and start recognizing it as a predictable, preventable, and reversible consequence of modern pharmacotherapy.
SOURCES
Bailey, R.L. et al. (2013). “Estimation of total usual calcium and vitamin D intakes in the United States.” Journal of Nutrition, 143(6), 825–831.
Brownie, S. (2006). “Why are elderly individuals at risk of nutritional deficiency?” International Journal of Nursing Practice, 12(2), 110–118.
Chaka, M. and Skrypnik, D. (2020). “Impact of long-term proton pumps inhibitor use on micronutrient status.” Nutrients, 12(3), 783.
De Jung, N. et al. (2003). “Nutritional status and health outcomes in elderly.” American Journal of Clinical Nutrition, 77(4), 1068–1074.
De Souza Ferreira, C. et al. (2021). “Polypharmacy and drug-nutrient interactions in older adults.” Frontiers in Pharmacology, 12, 660585.
Debase, J.K. et al. (2019). “Nutrient deficiency from long-term PPI use.” Mayo Clinic Proceedings, 94(12), 2404–2411.
Fairweather-Tait, S.J. et al. (2011). “Minerals in the aging population.” Journal of Nutrition, 141(4), 592–597.
Forman, J.P. et al. (2007). “Association between antihypertensive medication and risk of falls.” Journal of the American Geriatrics Society, 55(4), 590–595.
Gropper, S.S. and Smith, J.L. (2020). Advanced Nutrition and Human Metabolism. Engage Learning, 7th Ed.
Gupta, R. et al. (2022). “Motorman-associated vitamin B12 deficiency: Risk factors and screening.” Journal of Diabetes Research, 2022, 9672509.
Hubbard, R.E. and O’Mahony, M.S. (2009). “Drug-related adverse effects in older adults.” Therapeutic Advances in Drug Safety, 2(3), 103–112.
Institute of Medicine (IOM) (2011). Dietary Reference Intakes for Calcium and Vitamin D. The National Academies Press.
Kennedy, M. et al. (2023). “Micronutrient depletion in older adults using diuretics.” Clinical Nutrition ESPEN, 53, 156–162.
Klotz, U. (2009). “Pharmacokinetics and drug metabolism in the elderly.” Drug Metabolism Reviews, 41(2), 67–76.
Lichtenstein, A.H. et al. (2008). “Diet and lifestyle recommendations for cardiovascular disease risk reduction in the elderly.” Circulation, 117, 569–585.
López-Pintor, E. et al. (2018). “Xerostomia, hypo salivation and nutritional status.” Clinical Oral Investigations, 22(5), 1771–1780.
Maggie, D. et al. (2006). “Vitamin D status in the elderly: Implications for musculoskeletal health.” Aging Clinical and Experimental Research, 18(6), 447–452.
Manzoni, A.A. and Jackson, S.H.D. (2004). “Age-related changes in pharmacokinetics and pharmacodynamics.” British Journal of Clinical Pharmacology, 57(1), 6–14.
Morris, M.S. et al. (2005). “Foliate and vitamin B12 status and cognitive function in older adults.” American Journal of Clinical Nutrition, 82(3), 636–643.
Neuvonen, P.J. et al. (2006). “Drug interactions with food and nutrients.” Clinical Pharmacokinetics, 45(5), 347–365.
Roughed, Z.K. et al. (2009). “Calcium supplements and interactions with diuretics.” Journal of Clinical Pharmacology, 49(6), 678–686.
Saltzman, E. and Karl, J.P. (2013). “Nutritional considerations in older adults.” Nutrition in Clinical Practice, 28(5), 574–586.
Stops, S.J. et al. (2019). “Role of stations in coenzyme Q10 depletion.” Journal of Dietary Supplements, 16(5), 576–584.
HISTORY
Current Version
Aug 5, 2025
Written By:
ASIFA